Update: November 2018
The birth of a long-awaited baby is a joyful event, but not in all cases the birth ends successfully not only for the mother, but also for the child. One of these complications is fetal asphyxia, which occurs during childbirth. This complication is diagnosed in 4–6% of newly born children, and according to some authors, the frequency of newborn asphyxia is 6–15%.
Definition of newborn asphyxia
Translated from Latin, asphyxia means suffocation, that is, lack of oxygen. Asphyxia of newborns is a pathological condition in which gas exchange in the newborn’s body is disrupted, which is accompanied by a lack of oxygen in the child’s tissues and blood and the accumulation of carbon dioxide.
As a result, a newborn who was born with signs of a live birth either cannot breathe independently in the first minute after birth, or he experiences isolated, superficial, convulsive and irregular respiratory movements against the background of an existing heartbeat. Such children are immediately given resuscitation measures, and the prognosis (possible consequences) for this pathology depends on the severity of asphyxia, the timeliness and quality of resuscitation.
Classification of newborn asphyxia
Based on the time of occurrence, there are 2 forms of asphyxia:
- primary – develops immediately after the birth of the baby;
- secondary - diagnosed within the first day after birth (that is, at first the child was breathing independently and actively, and then suffocation occurred).
According to severity (clinical manifestations) there are:
- mild asphyxia;
- moderate asphyxia;
- severe asphyxia.
Factors provoking the development of asphyxia
This pathological condition is not an independent disease, but is only a manifestation of complications during pregnancy, diseases of the woman and the fetus. Causes of asphyxia include:
Fruit factors
- ) The child has;
- Rhesus conflict pregnancy;
- anomalies in the development of organs of the bronchopulmonary system;
- intrauterine infections;
- prematurity;
- intrauterine growth restriction;
- obstruction of the respiratory tract (mucus, amniotic fluid, meconium) or aspiration asphyxia;
- malformations of the heart and brain of the fetus.
Maternal factors
- severe, occurring against a background of high blood pressure and severe edema;
- decompensated extragenital pathology (cardiovascular diseases, diseases of the pulmonary system);
- pregnant women;
- endocrine pathology (, ovarian dysfunction);
- woman's shock during childbirth;
- disturbed ecology;
- bad habits (smoking, drinking alcohol, taking drugs);
- insufficient and malnutrition;
- taking medications contraindicated during gestation;
- infectious diseases.
Factors contributing to the development of disorders in the uteroplacental circle:
- post-term pregnancy;
- premature aging of the placenta;
- premature placental abruption;
- umbilical cord pathology (umbilical cord entanglement, true and false nodes);
- constant threat of interruption;
- and bleeding associated with it;
- multiple pregnancy;
- excess or lack of amniotic fluid;
- anomalies of labor forces (and incoordination, rapid and rapid labor);
- drug administration less than 4 hours before completion of labor;
- general anesthesia for women;
- uterine rupture;
Secondary asphyxia is provoked by the following diseases and pathologies in the newborn:
- impaired cerebral circulation in a child due to residual effects of damage to the brain and lungs during childbirth;
- heart defects that were not identified and did not appear immediately at birth;
- aspiration of milk or formula after a feeding procedure or poor-quality sanitation of the stomach immediately after birth;
- respiratory distress syndrome caused by pneumopathy:
- presence of hyaline membranes;
- edematous-hemorrhagic syndrome;
- pulmonary hemorrhages;
- atelectasis in the lungs.
Mechanism of development of asphyxia
It doesn’t matter what caused the lack of oxygen in the body of a newly born child, in any case, metabolic processes, hemodynamics and microcirculation are rebuilt.
The severity of the pathology depends on how long and intense the hypoxia was. As a result of metabolic and hemodynamic changes, acidosis develops, which is accompanied by a lack of glucose, azotemia and hyperkalemia (later hypokalemia).
In acute hypoxia, the volume of circulating blood increases, and in chronic and subsequent asphyxia, the blood volume decreases. As a result, the blood thickens, its viscosity increases, and the aggregation of platelets and red blood cells increases.
All these processes lead to microcirculation disorders in vital organs (brain, heart, kidneys and adrenal glands, liver). Disturbances in microcirculation cause swelling, hemorrhages and areas of ischemia, which leads to hemodynamic disturbances, disruption of the functioning of the cardiovascular system, and, as a consequence, all other systems and organs.
Clinical picture
 The main sign of asphyxia in newborns is considered to be respiratory failure, which entails a malfunction of the cardiovascular system and hemodynamics, and also impairs neuromuscular conduction and the severity of reflexes.
The main sign of asphyxia in newborns is considered to be respiratory failure, which entails a malfunction of the cardiovascular system and hemodynamics, and also impairs neuromuscular conduction and the severity of reflexes.
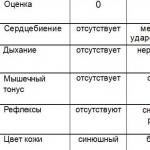
To assess the severity of the pathology, neonatologists use the Apgar assessment of the newborn, which is carried out in the first and fifth minutes of the child’s life. Each sign is scored 0 – 1 – 2 points. A healthy newborn gains 8–10 Apgar points in the first minute.
Degrees of newborn asphyxia
Mild asphyxia
With mild asphyxia, the number of Apgar points in a newborn is 6 - 7. The child takes the first breath within the first minute, but there is a weakening of breathing, slight acrocyanosis (cyanosis in the area of the nose and lips) and a decrease in muscle tone.
Moderate asphyxia
The Apgar score is 4 – 5 points. There is a significant weakening of breathing, possible disturbances and irregularity. Heartbeats are rare, less than 100 per minute, cyanosis of the face, hands and feet is observed. Motor activity increases, muscular dystonia develops with a predominance of hypertonicity. Possible tremor of the chin, arms and legs. Reflexes can be either reduced or enhanced.
Severe asphyxia
The condition of the newborn is serious, the number of Apgar scores in the first minute does not exceed 1 - 3. The child does not make breathing movements or takes separate breaths. Heart beats are less than 100 per minute, pronounced, heart sounds are dull and arrhythmic. The newborn does not cry, muscle tone is significantly reduced or muscle atony is observed. The skin is very pale, the umbilical cord does not pulsate, reflexes are not detectable. Eye symptoms appear: nystagmus and floating eyeballs, possible development of seizures and cerebral edema, DIC syndrome (impaired blood viscosity and increased platelet aggregation). Hemorrhagic syndrome (numerous hemorrhages on the skin) intensifies.
Clinical death
A similar diagnosis is made when all Apgar indicators are assessed at zero points. The condition is extremely serious and requires immediate resuscitation measures.
Diagnostics
When making a diagnosis: “Asphyxia of a newborn,” data from the obstetric history, how the birth proceeded, the child’s Apgar assessment at the first and fifth minutes, and clinical and laboratory tests are taken into account.
Determination of laboratory parameters:
- pH level, pO2, pCO2 (test of blood obtained from the umbilical vein);
- definition of base deficiency;
- level of urea and creatinine, diuresis per minute and per day (function of the urinary system);
- level of electrolytes, acid-base status, blood glucose;
- level of ALT, AST, bilirubin and blood clotting factors (liver function).
Additional methods:
- assessment of the functioning of the cardiovascular system (ECG, blood pressure control, pulse, chest x-ray);
- assessment of neurological status and brain (neurosonography, encephalography, CT and NMR).
Treatment
All newborns born in a state of asphyxia are given immediate resuscitation measures. The further prognosis depends on the timeliness and adequacy of treatment of asphyxia. Resuscitation of newborns is carried out using the ABC system (developed in America).
Primary care for a newborn
Principle A
- ensure the correct position of the child (lower the head, placing a cushion under the shoulder girdle and tilt it back slightly);
- suck out mucus and amniotic fluid from the mouth and nose, sometimes from the trachea (with aspiration of amniotic fluid);
- intubate the trachea and examine the lower respiratory tract.
Principle B
- carry out tactile stimulation - a slap on the baby’s heels (if there is no cry within 10 - 15 seconds after birth, the newborn is placed on the resuscitation table);
- jet oxygen supply;
- implementation of auxiliary or artificial ventilation (Ambu bag, oxygen mask or endotracheal tube).
Principle C
- performing indirect cardiac massage;
- administration of drugs.
The decision to stop resuscitation measures is made after 15–20 minutes if the newborn does not respond to resuscitation measures (there is no breathing and persistent bradycardia persists). Termination of resuscitation is due to the high probability of brain damage.
Administration of drugs
Cocarboxylase diluted with 10 ml of 15% glucose is injected into the umbilical vein against the background of artificial ventilation (mask or endotracheal tube). Also, 5% sodium bicarbonate is administered intravenously to correct metabolic acidosis, 10% calcium gluconate and hydrocortisone to restore vascular tone. If bradycardia appears, 0.1% atropine sulfate is injected into the umbilical vein.
If the heart rate is less than 80 per minute, indirect cardiac massage is performed with the mandatory continuation of artificial ventilation. 0.01% adrenaline is injected through the endotracheal tube (can be into the umbilical vein). As soon as the heart rate reaches 80 beats, cardiac massage stops, mechanical ventilation is continued until the heart rate reaches 100 beats and spontaneous breathing appears.
Further treatment and observation
After providing primary resuscitation care and restoring cardiac and respiratory activity, the newborn is transferred to the intensive care unit (ICU). In the intensive care unit, further treatment of asphyxia of the acute period is carried out:
Special care and feeding
The child is placed in an incubator, where constant heating is provided. At the same time, craniocerebral hypothermia is carried out - the newborn’s head is cooled, which prevents. Feeding of children with mild and moderate asphyxia begins no earlier than 16 hours later, and after severe asphyxia, feeding is allowed after 24 hours. The baby is fed through a tube or bottle. Breastfeeding depends on the baby's condition.
Prevention of cerebral edema
Albumin, plasma and cryoplasma, and mannitol are administered intravenously through the umbilical catheter. Drugs are also prescribed to improve blood supply to the brain (Cavinton, cinnarizine, vinpocetine, sermion) and antihypoxants (vitamin E, ascorbic acid, cytochrome C, aevit). Hemostatic drugs (dicinone, rutin, vikasol) are also prescribed.
Carrying out oxygen therapy
The supply of humidified and warmed oxygen continues.
Symptomatic treatment
Therapy is carried out aimed at preventing seizures and hydrocephalic syndrome. Anticonvulsants are prescribed (GHB, phenobarbital, Relanium).
Correction of metabolic disorders
Intravenous sodium bicarbonate is continued. Infusion therapy with saline solutions (saline and 10% glucose) is carried out.
Newborn monitoring
The child is weighed twice a day, the neurological and somatic status and the presence of positive dynamics are assessed, and the incoming and excreted fluid (diuresis) is monitored. The devices record heart rate, blood pressure, respiratory rate, and central venous pressure. From laboratory tests, a complete blood count with and platelets, acid-base status and electrolytes, blood biochemistry (glucose, bilirubin, AST, ALT, urea and creatinine) are determined daily. Blood clotting indicators and blood vessels are also assessed. cultures from the oropharynx and rectum. X-rays of the chest and abdomen, ultrasound of the brain, and ultrasound of the abdominal organs are indicated.
Consequences
Asphyxia of newborns rarely goes away without consequences. To one degree or another, the lack of oxygen in a child during and after childbirth affects all vital organs and systems. Particularly dangerous is severe asphyxia, which always occurs with multiple organ failure. The baby's life prognosis depends on the Apgar score. If the score increases in the fifth minute of life, the prognosis for the child is favorable. In addition, the severity and frequency of consequences depend on the adequacy and timeliness of resuscitation measures and further therapy, as well as on the severity of asphyxia.
Frequency of complications after suffering from hypoxia:
- in case of I degree of encephalopathy after hypoxia/asphyxia of newborns - the child’s development does not differ from the development of a healthy newborn;
- with stage II hypoxic encephalopathy – 25–30% of children subsequently have neurological disorders;
- with stage III hypoxic encephalopathy, half of the children die during the first week of life, and the rest, 75–100%, develop severe neurological complications with convulsions and increased muscle tone (later mental retardation).
After suffering asphyxia during childbirth, the consequences can be early and late.
Early complications
Early complications are said to occur when they appear during the first 24 hours of the baby’s life and, in fact, are manifestations of a difficult course of labor:
- cerebral hemorrhages;
- convulsions;
- and hand tremors (first small, then large);
- attacks of apnea (stopping breathing);
- meconium aspiration syndrome and, as a result, the formation of atelectasis;
- transient pulmonary hypertension;
- due to the development of hypovolemic shock and blood thickening, the formation of polycythemic syndrome (a large number of red blood cells);
- thrombosis (blood clotting disorder, decreased vascular tone);
- heart rhythm disorders, development of posthypoxic cardiopathy;
- disorders of the urinary system (oliguria, renal vascular thrombosis, swelling of the renal interstitium);
- gastrointestinal disorders (and intestinal paresis, digestive tract dysfunction).
Late complications
Late complications are diagnosed after three days of the child’s life and later. Late complications can be of infectious and neurological origin. The neurological consequences that appeared as a result of cerebral hypoxia and posthypoxic encephalopathy include:
- Hyperexcitability syndrome
The child has signs of increased excitability, pronounced reflexes (hyperreflexia), dilated pupils. There are no convulsions.
- Reduced excitability syndrome
Reflexes are poorly expressed, the child is lethargic and adynamic, muscle tone is reduced, dilated pupils, a tendency to lethargy, there is a symptom of “doll” eyes, breathing periodically slows down and stops (bradypnea, alternating with apnea), rare pulse, weak sucking reflex.
- Convulsive syndrome
Characterized by tonic (tension and rigidity of the muscles of the body and limbs) and clonic (rhythmic contractions in the form of twitching of individual muscles of the arms and legs, face and eyes) convulsions. Opercular paroxysms also appear in the form of grimaces, gaze spasms, attacks of unmotivated sucking, chewing and tongue protruding, and floating eyeballs. Possible attacks of cyanosis with apnea, rare pulse, increased salivation and sudden pallor.
- Hypertensive-hydrocephalic syndrome
The child throws back his head, the fontanelles bulge, the cranial sutures diverge, the head circumference increases, constant convulsive readiness, loss of function of the cranial nerves (strabismus and nystagmus are noted, smoothness of the nasolabial folds, etc.).
- Syndrome of vegetative-visceral disorders
Characterized by vomiting and constant regurgitation, disorders of intestinal motor function (constipation and diarrhea), marbling of the skin (spasm of blood vessels), bradycardia and rare breathing.
- Movement disorder syndrome
Residual neurological disorders (paresis and paralysis, muscle dystonia) are characteristic.
- Subarachnoid hemorrhage
- Intraventricular hemorrhages and hemorrhages around the ventricles.
Possible infectious complications (due to weakened immunity after multiple organ failure):
- development ;
- damage to the dura mater ();
- development of sepsis;
- intestinal infection (necrotizing colitis).
Question answer
Question:
Does a child who suffered birth asphyxia need special care after discharge?
Answer: Yes, sure. Such children need especially careful monitoring and care. Pediatricians, as a rule, prescribe special gymnastics and massage, which normalize the baby’s excitability and reflexes and prevent the development of seizures. The child must be provided with maximum rest, with preference given to breastfeeding.
Question:
When is a newborn being discharged from the hospital after asphyxia?
Answer: You should forget about early discharge (on days 2–3). The baby will be in the maternity ward for at least a week (an incubator is required). If necessary, the baby and mother are transferred to the children's department, where treatment can last up to a month.
Question:
Are newborns who have suffered asphyxia subject to dispensary observation?
Answer: Yes, all children who have suffered asphyxia during childbirth are required to be registered with a pediatrician (neonatologist) and neurologist.
Question:
What consequences of asphyxia are possible in an older child?
Answer: Such children are prone to colds due to weakened immunity, their performance at school is reduced, reactions to some situations are unpredictable and often inadequate, psychomotor development and speech lag are possible. After severe asphyxia, epilepsy, convulsive syndrome often develops, mental retardation is possible, and paresis and paralysis.
A woman walking the nations knows one thing, the most important thing for her is the importance of hearing the first cry of her newborn baby in the first minute after birth. We know that the faster and louder a child screams, the healthier he will be. In fact, a baby's cry is nothing more than a sign of physiological maturity. When the fetus is still in the womb, its glottis is tightly closed to prevent amniotic fluid from entering the respiratory system. Once the baby is born, his glottis is still closed. And the first cry of a newborn baby occurs due to exhalation from a narrowed gap.
It is a mistake to believe and trust folk superstitions that say that the first cry of a newborn baby is his attitude to everything that happens. Some grandmothers went so far in their predictions as to claim that a newborn baby cries at birth because he knows how hard life awaits him. These are just fables and they have no scientific basis.
Scientists claim that the cry of a newborn is not at all a signal of painful sensations. On the contrary, infants have no pain reactions at all for some period. It’s just that children are so savvy that they soon understand that screaming is the most effective way to attract the attention of their parents. So they take advantage of it.
To hear the cry of your baby immediately after his birth, you need to approach not only the birth process, but also the entire pregnancy with all responsibility. Unfortunately, few expectant mothers approach the birth process with full awareness of what is happening to her body, with an understanding of the physiology and psychology of childbirth. Most women rely on Mother Nature, hoping that she will do everything right. In fact, for pregnancy and childbirth to be successful, you need to prepare yourself for it in advance.
It is necessary to be especially careful in following all recommendations of obstetricians and gynecologists in the last weeks of pregnancy. This is the time that is given to you so that you can prepare yourself emotionally for the upcoming changes in your life. Finish all your work at work, rest more, try to improve your sleep and spend more time outdoors. Leading an unhealthy lifestyle, nervous shock, emotional distress, chronic lack of sleep are factors that can trigger premature birth. Premature babies are at greatest risk of harm to health in the first minutes of life, due to an inadequately formed respiratory system.
Take a responsible approach to examining your health and the health of the future dad before conception. The percentage of children contracting various infections from their mother during the birth process is enormous. Infections penetrate the defenseless and fragile infant body during passage through the birth canal. And if for the mother the bacteria could be absolutely harmless, then for the newborn they are dangerous and aggressive. Note that almost all children become infected with various infections during childbirth, but a full-term healthy baby can easily cope with illnesses, while for a premature baby, a mild infection can cause irreparable harm to health and become a serious threat to his life.
Throughout your pregnancy, be observed by an experienced doctor, follow all recommendations, attend special courses and trainings for future parents that will teach you how to cope with pain during childbirth. And then you can fully enjoy the loud, healthy first cry of your newborn baby.
The main biological significance of this cry-cry is to prevent separation of mother and child in the first hours after birth. This is the main reason why a baby cries after childbirth.
For a newborn baby, crying is the only available way in which he can communicate to his mother about his needs before gaining the gift of speech. The baby's first cry is a plea for protection, a reaction of fear and discomfort when entering a new, unfamiliar and not very friendly environment.
What the child experiences during the process and in the first moments after birth can be compared to the sensations of a person who suddenly falls through the ice: loss of orientation, cold, difficulty breathing. Add to this the feeling of compression when passing through the birth canal, and all this - after 9 months in the usual warm and cozy “house”. That is why, in most modern maternity wards, they practice putting the baby to the breast immediately after birth (if there is no threat to the health of the baby and mother). The baby calms down, feeling the warmth of his own body, hearing the familiar sounds of his mother’s heart and his mother’s gentle voice.
An amazing fact: for quite a long time - up to six months after birth, and more - children often cry without tears. Especially at night. The child seems to continue to sleep - his eyes are closed and there are no tears in them. This is not a cry of pain or resentment. Simply, with the help of various intonations, the little man communicates some of his needs. A sensitive mother gradually begins to distinguish between different types of crying. For example, it has been noticed that in pain, a child, as a rule, emits rather sharp, piercing screams with “bays”, while a hungry cry is more monotonous, begins with whimpering sounds and increases over time.
The main reasons for crying in babies of the first year of life are most often: hunger, pain (the most common problem is intestinal colic and teething), uncomfortable ambient temperature, skin irritation from wet diapers, fatigue, anger (for example, as a response to restriction of freedom movements); In addition, the baby may simply be sad and lonely.
In the minds of many parents, to this day, various myths about children's crying live, supposedly while crying, the child “develops his lungs” or “strengthens his character.” However, recently, psychologists are inclined to believe that there is nothing useful for a baby in prolonged crying. Rather, on the contrary: if the mother does not come for a long time, the little man experiences increased stress - after all, his fragile world is left without protection. This can have a negative impact on the child's psyche. Moreover, a heart-rending cry “until you turn blue” can cause harm, even on a physiological level: cause oxygen starvation, or pathological conditions of the respiratory system. Young parents often worry whether they will spoil their child by reacting to every cry. Experts say: for children under one year old, there can be no talk of any “pampering”. The parents' quick response to the child's needs gives him a feeling of security and comfort, which contributes to his harmonious development.
Now you understand why it is normal for a baby to cry after giving birth. Now let's talk about how to calm a crying newborn?
First- offer food. "Baby" best soothes mother's breasts. There are many reasons for this: the frequent need for nutrition, the familiar mother’s smell, and the warmth of the mother’s body. The modern method of “free” breastfeeding encourages the baby to attach to the breast every time he shows concern. If breastfeeding is not possible, the mother should bottle-feed the baby, hugging him and lightly pressing him to her body. After finishing feeding, you can give the child a pacifier: children who are bottle-fed need satisfaction of the sucking reflex more than others.
Second- you need to make sure that the baby’s delicate skin does not experience discomfort - a dirty and wet diaper, or a diaper that has bunched up under the back can cause irritation. In addition, babies do not tolerate heat and cold well. Therefore, parents should often check whether the child’s clothes and bedding are in order. And monitor how comfortable the air temperature in the room is. You should also make sure that the baby does not get hurt by his own sharp nails - anti-scratch mittens are a great way to save from such troubles.
Third- carry out a set of procedures to eliminate intestinal colic. Currently, pharmacies offer a wide range of drugs that relieve colic. But, no one has canceled the “old-fashioned” methods: dill water, laying on the tummy, “dry heat”, a light soothing massage - all this can greatly make life easier for the little man and his parents. And, of course, for a breastfeeding mother, a special diet is required that excludes cabbage, peas, sweet fruits, and other foods that contribute to gas formation in the intestines.
Fourth The method is as old as the world, but its reliability is not in doubt: you need to carry the baby in your arms, rocking it slightly. You can use a “sling” - this becomes especially relevant when the baby’s weight exceeds five kilograms.
Fifth- sing a lullaby, or just talk to him gently. Mom's affectionate voice is a great soothing voice.
Sixth. Many children, from the age of three months, begin to worry about teething. Therefore, it is worth stocking up on various teethers and pain-relieving gel in advance. Teethers with a cooling effect are very effective.
Seventh. It’s rare, but it still happens that none of the above (and many other) methods give results. The baby cries for a very long time and does not intend to stop. Take a closer look at his physiological reactions. Perhaps the crying is associated with some serious illness. In this case, the best thing is to consult a doctor.
Eighth, and most importantly - don't get annoyed. Always remember that a newborn baby does not cry to disturb your sleep or test your patience. He still simply doesn’t know how to cry “out of spite.” The excited state and negative attitude of parents are easily transmitted to the baby. And, in the same way, the calmness and goodwill of the mother is “absorbed” by the child, which helps him fall asleep as quickly as possible.
05-01-2008, 23:31
05-01-2008, 23:34
Mine didn’t scream right away either. They performed special actions on her, after which she screamed! Developing well! Experts don’t see any pathologies! We do vaccinations according to schedule, as expected, there are no problems after them! Ttt
05-01-2008, 23:36
When my daughter was born, they cut the umbilical cord, but she didn’t scream right away. I remember the pediatrician took her, examined her (slowly), then took her somewhere and a few minutes later I heard my baby scream. My waters were meconium, Apgar 7/8. When I asked later, the pediatrician replied that it was good that she didn’t scream right away, otherwise she would have swallowed meconium. And I’m worried that something might be wrong with my daughter in the future. Who had the same situation. Which specialists should I show it to? What should you pay attention to? I read somewhere that such children should be vaccinated under the supervision of an immunologist, but we will soon receive DTP. I'm really looking forward to answers
Vaccinations for any children should be approached with caution and attentiveness.
The very fact that the child did not cry means nothing. He doesn't have to yell at all. I groaned and it was wonderful. I didn't scream.
Special observation based on this fact alone is definitely not required.
05-01-2008, 23:37
My son didn’t scream right away either. He lay quietly on his stomach. And then, when the pediatrician took him away, only then did he scream. When he was lying on his stomach, I asked why he wasn’t crying. The obstetrician and pediatrician just smiled and said that everything was fine, the child was healthy, on a scale of 8/9.
Now he is 9.5 months old. It's okay, TTT
05-01-2008, 23:39
When my daughter was born, they cut the umbilical cord, but she didn’t scream right away. I remember the pediatrician took her, examined her (slowly), then took her somewhere and a few minutes later I heard my baby scream. My waters were meconium, Apgar 7/8. When I asked later, the pediatrician replied that it was good that she didn’t scream right away, otherwise she would have swallowed meconium. And I’m worried that something might be wrong with my daughter in the future. Who had the same situation. Which specialists should I show it to? What should you pay attention to? I read somewhere that such children should be vaccinated under the supervision of an immunologist, but we will soon receive DTP. I'm really looking forward to answers
Maybe I just had meconium in my mouth and couldn’t scream. They cleaned their mouth and nose and screamed immediately. This is not always an indicator. Most likely, nothing will happen after this, but if you are worried, just bring this to the attention of a neurologist, so that he can take a closer look and not miss anything. Everything should be fine.
05-01-2008, 23:46
This was the first spanking...
05-01-2008, 23:53
Mine didn't scream either. The doctor said that this is normal. It is enough for her to make at least some sounds (groaning, coughing, etc.). So air passes through - breathes...
This was the first spanking...
+1
They didn’t even let us scream. They put me on my stomach, and he started snoring contentedly :)
Masenka
06-01-2008, 00:02
My daughter didn’t scream right away either. Until they began to process and dress her, she remained silent. Apgar score 8/9. The pediatrician and midwife said we were both tired from labor. When he rests, he screams. And so it happened :)) We even have photographic evidence. All my friends are surprised. Sometimes it seems to me that after she was born, she looked around, she liked everything, and she did not find a reason to cry. ;) All specialists are happy with us (TTT) Don’t worry. IMHO If she had not screamed due to asphyxia or other problems, you would have been informed immediately. And the problems would have already appeared. Your daughter just liked you and decided not to cry :)
06-01-2008, 00:19
Mine screamed after 3 minutes. She is completely healthy.
06-01-2008, 09:50
Apgar score 8/9. The pediatrician and midwife said we were both tired from labor. When he rests, he screams.
:010::010::010:
Which specialists should I show it to? What should you pay attention to? I read somewhere that such children should be vaccinated under the supervision of an immunologist, but we will soon receive DTP. I'm really looking forward to answers
1. None.
2. no matter what
3. that's not true
Summary: Your child suffered mild asphyxia during childbirth. Now he is a child like everyone else. Do not worry.
Elena Malysheva
06-01-2008, 12:25
He didn’t scream right away.
They didn’t do DPT at 3 months, the neurologist gave me a medical referral.
06-01-2008, 13:53
the situation is similar. Only we had another 3rd umbilical cord entanglement. They observe it like all children.
06-01-2008, 14:01
Now he is a foal like everyone else.
:)):)):))
06-01-2008, 14:24
Mine didn’t scream right away either, they plopped her down on her stomach, she was silent, then they took her in for treatment, that’s when we started screaming... Apgar 7/8, the neurologist didn’t see any abnormalities in a month...
06-01-2008, 14:27
All my children did not cry at once, my son with a double entanglement of the umbilical cord, my daughter and second son - large and fast births - but everyone is developing normally, and there are no deviations of any kind....
Neonatal asphyxia is a clinical symptom in which a child immediately after birth does not have spontaneous breathing and oxygen does not reach the brain. Normally, a newborn should take his first breath and cry almost immediately as he is born, but sometimes this does not happen for various reasons. Severe asphyxia can cause permanent damage to a baby's brain, so it is extremely important to prevent it and treat it as quickly as possible.
Asphyxia is closely related to birth trauma in the baby. A large number of children with such consequences of asphyxia, such as delayed psychomotor development, stunted growth, poor academic performance, low or high tone, hearing and vision impairment, pass through our center every month. Although many of these children can be helped by osteopathy, it is much better if asphyxia could be avoided altogether.
The happiness of an osteopathic doctor, as well as of parents, would be if all children were born absolutely healthy. Simple rules of prevention during pregnancy and before childbirth can dramatically reduce the likelihood of complications in the child and prevent such undesirable phenomena as asphyxia and its consequences. It is much easier and more pleasant to prevent a disease than to treat its complications.
Symptoms of asphyxia in a newborn
Depending on the severity of asphyxia, it is customary to distinguish three degrees: mild, moderate and severe. The assessment of the condition is expressed in Apgar scores.
- Mild asphyxia (Apgar score 6-7) – the baby takes his first breath within a minute after birth. Breathing is weak, lips, arms and legs may be blue, muscles and tone are flaccid.
- Moderate severity (4-5 Apgar points) - about a minute passes from birth to the first breath. Breathing is weak, irregular, the cry is quiet and sluggish, the pulse is rare. The muscle tone is low, the limbs and face are blue, but the umbilical cord retains its pulsation.
- Severe asphyxia (1-3 points) – there is no breathing, or the child breathes irregularly and weakly, does not cry. The heart rate is very slow, the umbilical cord does not pulsate. The skin is pale.
How and why asphyxia develops during childbirth
In the womb, the baby cannot breathe through the lungs; their role is played by the placenta. Until the very moment of birth, the child depends on how well the blood is saturated with oxygen in the placenta and flows to his brain. Any obstruction in this area can cause fetal asphyxia:
- Umbilical cord entanglement - the vessels inside the umbilical cord are compressed, blood flows poorly from the placenta to the fetus.
- Premature placental abruption - oxygen does not flow from the mother to the placenta, the child does not receive it for a long time, since blood circulation in the placenta is impaired.
- Very long labor and weak labor also reduce the flow of oxygen to the baby’s brain, which can result in asphyxia.
After birth, asphyxia can be caused by blockage of the baby's airways with mucus, meconium, or amniotic fluid.
The risk of asphyxia increases if the expectant mother has heart disease, anemia, diabetes mellitus, or suffered an infectious disease on the eve of childbirth. A clinically narrow pelvis, a long anhydrous period during childbirth, oligohydramnios and other pregnancy problems also contribute to the development of asphyxia.
Consequences of newborn asphyxia
Short-term asphyxia does not cause irreversible damage to the child’s brain, since his body is adapted for this. However, prolonged oxygen starvation can cause the death of cortical neurons, which will certainly make itself felt in the future.
The consequences of severe asphyxia are considered to be disturbances in the mental and motor development of the child, late onset of walking and speech, developmental delays, cortical visual and hearing impairments - a whole range of serious diseases that can be prevented by simple prevention.
Treatment and prevention of asphyxia in newborns
Treatment of severe asphyxia should begin immediately after birth. To do this, the child is sucked out of the mucus from the respiratory tract, stimulated breathing with special techniques, and given oxygen. In the most severe cases, resuscitation incubators for newborns are used.
Our doctors have extensive experience working with expectant mothers, constantly improve their skills through advanced training courses, and attend scientific symposia on the problems of osteopathic care for pregnant women and infants. From experience, we can say for sure that careful preparation for childbirth, including osteopathy, significantly reduces the risk of complications and asphyxia during childbirth, guaranteeing the safe birth of your baby and good development in the future.